Ancient medicine: how was illness treated in the Greco-Roman era?
The roots of modern medicine can be traced back to the pioneering practices of our classical forebears. Let’s take a step back in time and explore the remedies and procedures used at that time.
Medicine in ancient Greece and Rome
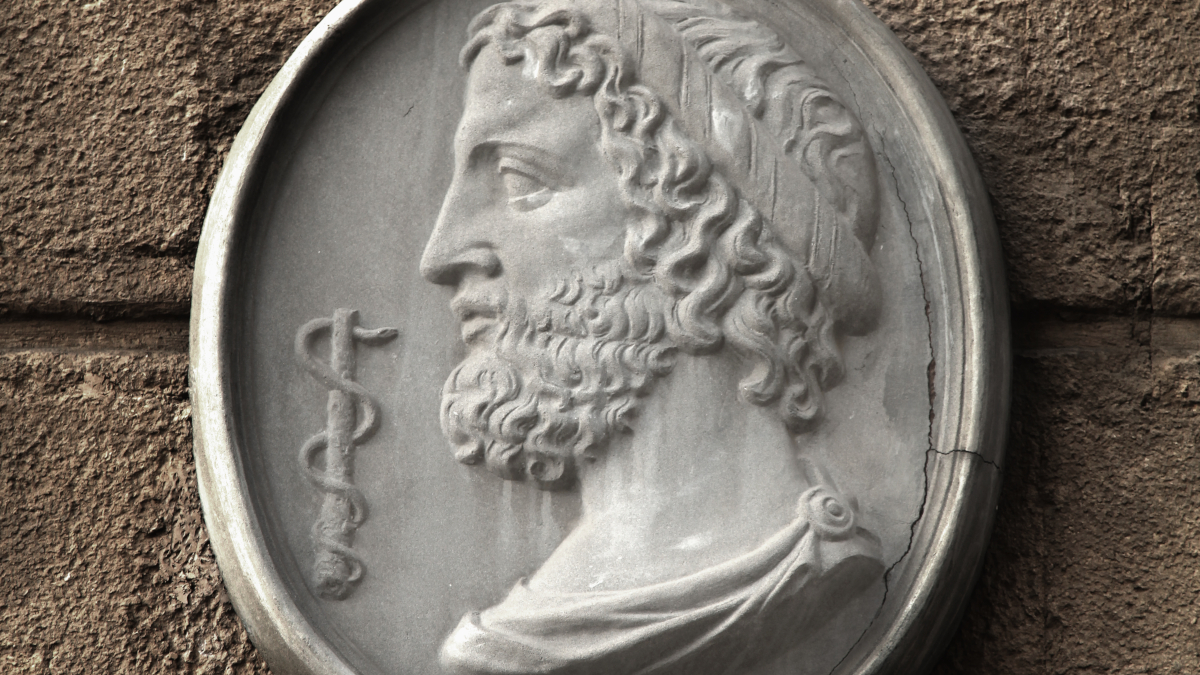
For a long time, medicine retained a certain mystical dimension. Illness was commonly seen as an expression of divine anger which had to be silenced at all costs. Thus treatments mainly took the form of incantations, ablutions, purifications and offerings, presided over by priest-doctors in special sanctuaries (like that of the God of Medicine, Asclepius, in Epidaurus).
In Greece, the first person to eschew any consideration of deities in the practice of medicine was Hippocrates (460 BC-377 BC) who gave his name to the ethical oath still taken today by young Western medics (1).
Medical knowledge, which had hitherto not been rooted in any teaching, then became structured around the Library of Alexandria around 285 BC. This great institution housed the most important treatises on medicine from the Eastern Mediterranean, and was considered a major research center. It spawned eminent figures such as Herophilos, Celsus and Dioscorides.
Though it differed from Greek practices, Roman medicine initially took its lead from the Greeks in that people prayed to their gods to ward off plagues. Medicine was practised in temples as well as in private clinics (iatreia) or by itinerant doctors. Some had their own specialties such as treating gladiators wounded in combat, or were affiliated to guilds or colleges in clinic-like settings (schola), and military hospitals (valetudinaria) also came into being.
De materia medica from Dioscorides: ancient use of medicinal plants
Born around the year 25 BC, Dioscorides is today regarded as the father of pharmacology. His work De materia medica, used by apothecaries until the 16th century, lists more than 800 mainly plant substances (2).
Combining his experience as a doctor, pharmacologist and botanist, he proceeded to painstakingly classify the ‘simples’ (the old name for medicinal plants), listing their names, species, geographical origins, parts used, preparations and methods of administration. Therapeutic indications and dosages were all carefully detailed in his pharmacopoeia (3).
Plants, fruits and flowers were prepared in multiple forms: the more familiar herbal teas (infusions, decoctions…), but also herbal baths and enemas, powders, pastes and plasters.
At that time, camomile, rue and saffron were considered effective at regulating the menstrual cycle (4-5). Castor oil was used as a laxative (6), fennel was popular for its diuretic properties (7), while pomegranate was believed to eradicate tapeworm (8). Widely consumed as a spice by the Greeks and Romans, ginger was much-praised for its digestive benefits (9).
And even then, willow bark had been identified as a natural ‘aspirin’, validated by its effective salicylic acid content (10).
The place for animals and minerals in ancient medicine
In ancient times, animals were involved in the healing process in one of two ways: either by taking on the ill person’s sickness (acting as a scapegoat), or by providing therapeutic substances.
Though butter, beehive products (such as honey and royal jelly) and milk are the best-known examples of these, other far more unusual remedies – more magical than scientific – are mentioned in the literature, such as cobwebs or hare and sheep droppings (11). Of these unlikely therapies, only castoreum (secreted by beavers) really proved its worth: it was prized by our ancient forebears for treating epilepsy, fever, headaches and uterine pain.
In terms of minerals, iron salts were mentioned by Dioscorides as being powerful haemostatics able to stem the flow of blood from wounds (12). Indeed, the image on many Greek vases of Achilles rubbing the rust of his spear onto Telephus’ wound would appear to confirm the ancient origins of this discovery.
And mercury, copper, lead and sulfur salts had many applications in ophthalmology. Combined with various plant extracts, box leaves, celandine or rosemary, they were used to form pressed tablets or cakes of paste which were then scraped or diluted and used for treating eye discharge, burning or suppuration (13-14).
The basics of mycology
Rarely studied before the 17th century, mushrooms make a modest appearance in the writings of Pliny and Dioscorides. De materia medica devotes a paragraph to agarikon, also known as larch polypore.
Regarded by the Ancient Greeks as the elixir of long life, this wood-decay fungus was defined therein as ‘astringent’ and ‘warming’ (15-16). Its entry states that it offers remarkable efficacy against “all internal conditions if given taking account of effect and age, one with water, the other with wine, with sour honey or mead”.
Surgical procedures in ancient times
Archaeological digs carried out at the site of Pompeii have revealed an extraordinary variety of surgical instruments: lancet, scalpel, hook, cautery, forceps, ventouse, syringe, trephine…
While it is difficult to place these elements in context, evidence suggests that Greco-Roman practitioners mastered the intricacies of many surgical procedures. These ranged from the relatively simple fracture fixation by ‘resetting’ bones, to more complex visceral surgery and tricky cataract operations. Equally remarkable were the creation of fully-functional dentures (made from gold during the Etruscan period) to replace teeth that had been damaged most often by millstone residues inadvertently left in bread.
And how did they put patients to sleep? In the absence of actual anaesthesia, doctors used sedative drinks. While decoctions made from hemp and opium were used abundantly in Eastern Antiquity, the Romans preferred wine or alcohol mixed with various plants such as belladonna, poppy juice, Indian hemp or mandrake (17-19), even though some of these, such as aconite, posed a serious risk to the patient regaining consciousness (20)…
SuperSmart ADVICE
References
- Tsiompanou E, Marketos SG. Hippocrates: timeless still. J R Soc Med. 2013 Jul;106(7):288-92. doi: 10.1177/0141076813492945. PMID: 23821709; PMCID: PMC3704070.
- Staub PO, Casu L, Leonti M. Back to the roots: A quantitative survey of herbal drugs in Dioscorides' De Materia Medica (ex Matthioli, 1568). Phytomedicine. 2016 Sep 15;23(10):1043-52. doi: 10.1016/j.phymed.2016.06.016. Epub 2016 Jun 23. PMID: 27444350.
- Yarnell E, Touwaide A. Accuracy of Dioscorides,' De materia medica (First Century C.E.), Regarding Diuretic Activity of Plants. J Altern Complement Med. 2019 Jan;25(1):107-120. doi: 10.1089/acm.2018.0251. Epub 2018 Nov 7. PMID: 30403493.
- Niazi A, Moradi M. The Effect of Chamomile on Pain and Menstrual Bleeding in Primary Dysmenorrhea: A Systematic Review. Int J Community Based Nurs Midwifery. 2021 Jul;9(3):174-186. doi: 10.30476/ijcbnm.2021.87219.1417. PMID: 34222539; PMCID: PMC8242407.
- Rajabi F, Rahimi M, Sharbafchizadeh MR, Tarrahi MJ. Saffron for the Management of Premenstrual Dysphoric Disorder: A Randomized Controlled Trial. Adv Biomed Res. 2020 Oct 30;9:60. doi: 10.4103/abr.abr_49_20. PMID: 33457343; PMCID: PMC7792881.
- Polito L, Bortolotti M, Battelli MG, Calafato G, Bolognesi A. Ricin: An Ancient Story for a Timeless Plant Toxin. Toxins (Basel). 2019 Jun 6;11(6):324. doi: 10.3390/toxins11060324. PMID: 31174319; PMCID: PMC6628454.
- Badgujar SB, Patel VV, Bandivdekar AH. Foeniculum vulgare Mill: a review of its botany, phytochemistry, pharmacology, contemporary application, and toxicology. Biomed Res Int. 2014;2014:842674. doi: 10.1155/2014/842674. Epub 2014 Aug 3. PMID: 25162032; PMCID: PMC4137549.
- Pawlowski ZS. Role of chemotherapy of taeniasis in prevention of neurocysticercosis. Parasitol Int. 2006;55 Suppl:S105-9. doi: 10.1016/j.parint.2005.11.017. Epub 2005 Dec 13. PMID: 16356763; PMCID: PMC7108384.
- Nikkhah Bodagh M, Maleki I, Hekmatdoost A. Ginger in gastrointestinal disorders: A systematic review of clinical trials. Food Sci Nutr. 2018 Nov 5;7(1):96-108. doi: 10.1002/fsn3.807. PMID: 30680163; PMCID: PMC6341159.
- Mahdi JG, Mahdi AJ, Mahdi AJ, Bowen ID. The historical analysis of aspirin discovery, its relation to the willow tree and antiproliferative and anticancer potential. Cell Prolif. 2006 Apr;39(2):147-55. doi: 10.1111/j.1365-2184.2006.00377.x. PMID: 16542349; PMCID: PMC6496865.
- Bagameri L, Baci GM, Dezmirean DS. Royal Jelly as a Nutraceutical Natural Product with a Focus on Its Antibacterial Activity. Pharmaceutics. 2022 May 27;14(6):1142. doi: 10.3390/pharmaceutics14061142. PMID: 35745715; PMCID: PMC9227439.
- Solc MK, Weese JS, Jazic E. The in vitro antibacterial activity of incomplete iron salt of polyacrylic acid against Pseudomonas aeruginosa, meticillin-resistant Staphylococcus pseudintermedius and meticillin-resistant S. aureus. Vet Dermatol. 2018 Feb;29(1):3-e2. doi: 10.1111/vde.12483. Epub 2017 Aug 22. PMID: 28833656.
- de Oliveira JR, Camargo SEA, de Oliveira LD. Rosmarinus officinalis L. (rosemary) as therapeutic and prophylactic agent. J Biomed Sci. 2019 Jan 9;26(1):5. doi: 10.1186/s12929-019-0499-8. PMID: 30621719; PMCID: PMC6325740.
- Gilca M, Gaman L, Panait E, Stoian I, Atanasiu V. Chelidonium majus--an integrative review: traditional knowledge versus modern findings. Forsch Komplementmed. 2010 Oct;17(5):241-8. doi: 10.1159/000321397. Epub 2010 Oct 8. PMID: 20980763.
- Girometta C. Antimicrobial properties of Fomitopsis officinalis in the light of its bioactive metabolites: a review. Mycology. 2018 Oct 25;10(1):32-39. doi: 10.1080/21501203.2018.1536680. PMID: 30834150; PMCID: PMC6394315.
- Jakopovic B, Oršolić N, Kraljević Pavelić S. Antitumor, Immunomodulatory and Antiangiogenic Efficacy of Medicinal Mushroom Extract Mixtures in Advanced Colorectal Cancer Animal Model. Molecules. 2020 Oct 28;25(21):5005. doi: 10.3390/molecules25215005. PMID: 33126765; PMCID: PMC7663060.
- Lee FC, Holt SK, Hsi RS, Haynes BM, Harper JD. Preoperative Belladonna and Opium Suppository for Ureteral Stent Pain: A Randomized, Double-blinded, Placebo-controlled Study. Urology. 2017 Feb;100:27-32. doi: 10.1016/j.urology.2016.07.035. Epub 2016 Sep 19. PMID: 27658661; PMCID: PMC5448974.
- Chidiac EJ, Kaddoum RN, Fuleihan SF. Special article: mandragora: anesthetic of the ancients. Anesth Analg. 2012 Dec;115(6):1437-41. doi: 10.1213/ANE.0b013e318259ee4d. Epub 2012 May 14. PMID: 22584550.
- Houghton IT. Some observations on early military anaesthesia. Anaesth Intensive Care. 2006 Jun;34 Suppl 1:6-15. doi: 10.1177/0310057X0603401S01. PMID: 16800222.
- Chan TY. Aconite poisoning. Clin Toxicol (Phila). 2009 Apr;47(4):279-85. doi: 10.1080/15563650902904407. PMID: 19514874.
Keywords
5 Days
great products and prices
great products and prices
Marie
11 Days
Easy to navigate site
Easy to navigate site, had what I was searching for, good price. easy order-check out
James Tucker
17 Days
My skin is clearing up nicely!
Pretty good for my skin so far.
Christian
19 Days
The new packaging is excellent
The new packaging is excellent - finally! No more squashed boxes and torn envelopes.
GORAN
20 Days
Great Product
Great Product
Larry Garrett
24 Days
Quick shipping
Quick shipping; good price. No issues!
Mary McCarty
26 Days
Thr product is very good and is helping…
Thr product is very good and is helping me on my health. Then is always on time
LUGO Luz
28 Days
Buying was fine
Buying was fine. I had problems with the website not recognizing my login info, and had to call to get it fixed. Other than that, everything was good.
David S. Clark
29 Days
Your super maca and super ginseng are…phenomenal
Your super maca and super ginseng are phenomenal supplements that compliment each other when taking them together. Fantastic feeling of well-being and lots of mid day energy without the crash.
Keith Mason
31 Days
I have had amazing results with every…
I have had amazing results with every supplement I've purchased. I am extremely satisfied with this company
kirstin Torres
31 Days
Fine products
Fine products . They are on the leading edge of online supplements. The only issue -so far-is they sometime run out of subscription items.
Jason Argos
34 Days
The ordering process is very user…
The ordering process is very user friendly and the products always come in a timely manner.
CARTER Rhonda
35 Days
The price for Dr
The price for Dr. Pero's AC-11 is reasonable and in line with his views. (my former colleague). Keep it pure.
CAMPBELL Clayton
38 Days
Right on every time.
Right on every time.
Arthur Nicholas
41 Days
They are cheaper than everyone else and…
They are cheaper than everyone else and the shipping was fast. Great company.
Patricia Adams